Why do we have problems with the oral cavity?
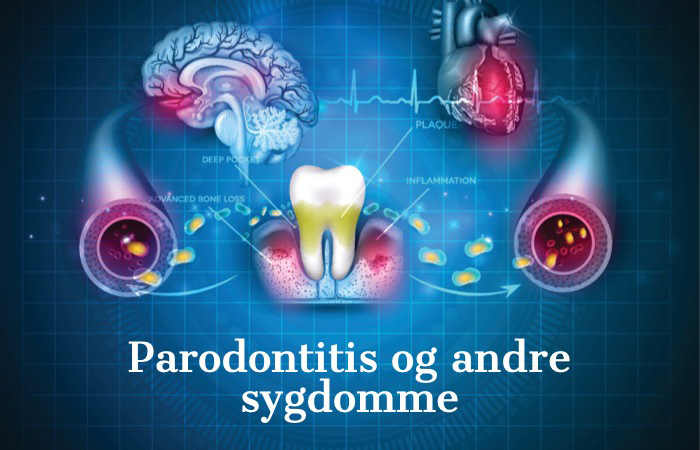
It's not just our teeth that need to be strong and healthy, the mucous membranes are just as important to our health, and not just in the oral cavity, but to our health throughout the body. That's why there's more focus on a healthy mouth and the many factors that come into play when we have problems in the oral cavity. Recent studies show that the composition of the biofilm in the oral cavity has a severe impact on our overall health. Four key factors affect your oral cavity and, in turn, your body.

Healthy mouth – healthy body
Why do we have problems with the oral cavity?
There are several factors of importance when we develop problems in the oral cavity. It is well known that good oral hygiene and preventive measures are crucial in determining whether we develop oral cavity disease. Fewer know that there are far more factors of importance to maintaining a healthy mouth.
The dental check-up - The way to a better health
Why do your patients have problems with the oral cavity?
There are several factors at play when your patients develop oral cavity problems. While good oral hygiene is essential and it is well known that preventive efforts are important in determining whether a patient develops an oral disease, this factor alone does not determine the onset and course of the disease.

CMS Dental No.1 in treatment through biofilm control in the oral cavity. We produce high quality equipment and products for the dental industry